Understanding Cervicogenic Headaches and the Role of Spine Instability
Introduction:
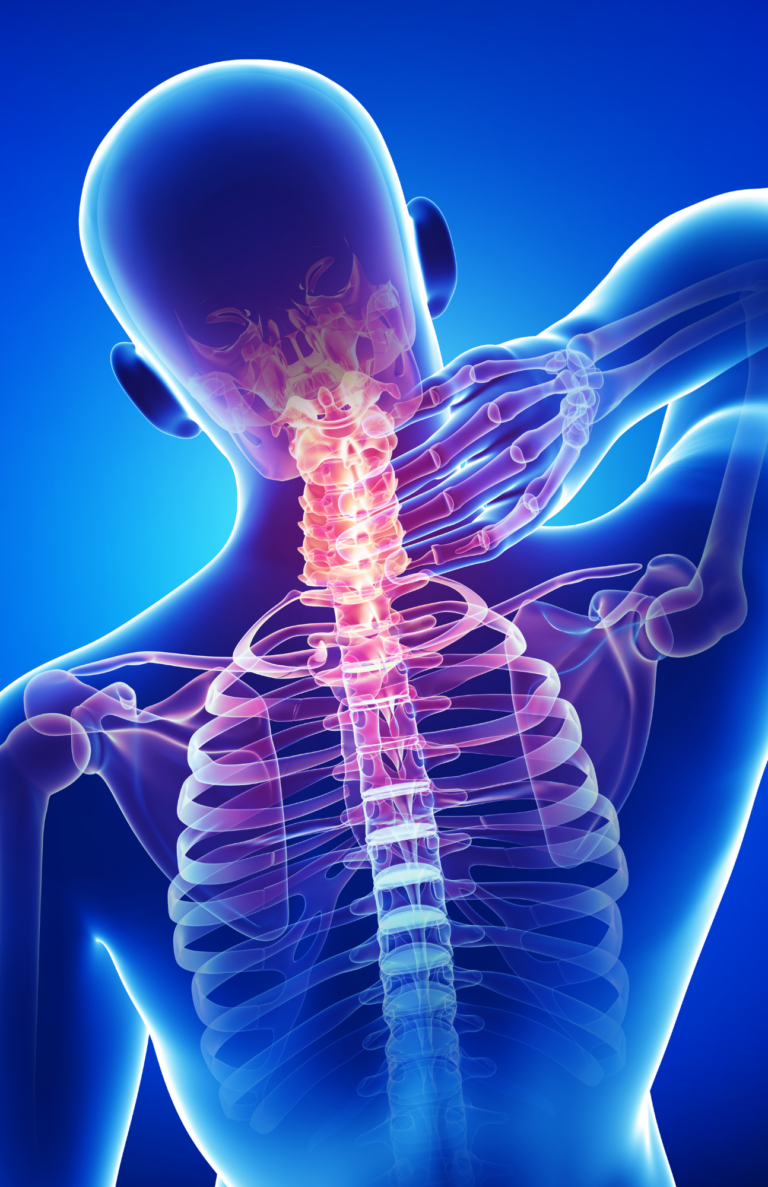
Headaches suck. They can and will stop your day if you don’t treat the cause. If you are having repetitive headaches, especially if you notice any pain at the back of the head and top of neck, maybe even with some tenderness of the muscles at the back of head, you are likely to have a cervicogenic headache. These headaches can often be diagnosed as migraine, since they can have overlapping features.
Understanding Cervicogenic Headaches:
Cervicogenic headaches are secondary headaches, meaning they are caused by an underlying condition or issue. Unlike migraines or tension headaches, cervicogenic headaches stem from structural problems in the neck or cervical spine. The pain typically originates from the upper cervical vertebrae and radiates to the back of the head, temples, forehead, and even the eyes. There can be cases of eye pain and redness, and even tooth or jaw pain if the trigeminal nerve distribution becomes involved.
Spine Instability and Cervicogenic Headaches:
Spinal instability means that loosened ligaments of the spine allow abnormal motion. It does not take injury or accidents to loosen ligaments. The term “creep” doesn’t just refer to that weirdo down the street, it is also the name of the process of slow ligament loosening. Every day with our repetitive motions we gradually strain the ligamentous tissues, and over years abnormal motion occurs. Of course this sort of thing can be caused or initiated by accidents etc., with things like whiplash or concussion being recognized initiators of headaches.
When the cervical spinal ligaments are loosened and abnormal motion occurs, multiple things happen. First is tightness of the muscles which overly the spine – this is a protective measure, where the muscles are attempting to stabilize the region. A very common story I hear from patients is how they have uncomfortable muscle tightness, so they get a massage. This makes them feel good for a day or so, and then they have new issues, sometime headaches, sometime numbness in the arm, which often start a few days after the massage. The reason this happens is that while the muscular tightness is uncomfortable, it is protective. When the massage loosens the muscles and removes the protection, the spinal instability can lead to compression or stretch of nerves, causing worsening or new symptoms.
Signs of Spine Instability:
- Neck Pain: Individuals with cervicogenic headaches often experience chronic neck pain that worsens with certain movements or positions.
- Crepitus: Cracking, rice crispy like sounds with movement of the neck, often that only the person themselves can hear.
- Reduced Range of Motion: Spine instability can restrict neck movement, leading to stiffness and difficulty turning the head.
- Muscle Tension: The surrounding muscles may become tense and tender, contributing to headache symptoms.
- Headache Triggers: Certain activities, such as prolonged sitting, poor posture, or neck movements, can trigger or exacerbate cervicogenic headaches.
Treatment Approaches:
- Physical Therapy: Physical therapy plays a vital role in stabilizing the cervical spine. Therapists can provide exercises to strengthen the neck muscles, improve posture, and enhance stability, helping to alleviate cervicogenic headaches.
- Manual Therapy: Techniques such as spinal manipulation, mobilization, and soft tissue manipulation can help restore proper alignment and relieve pressure on the nerves, reducing headache symptoms.
- Postural Correction: Correcting poor posture habits and ergonomics can help alleviate spine instability and reduce cervicogenic headaches. Maintaining a neutral spine position while sitting, standing, and engaging in activities can significantly impact headache frequency and intensity.
- Supportive Devices: In some cases, a supportive cervical collar or brace may be prescribed to provide stability and limit excessive motion in the cervical spine.
- Prolotherapy: Prolotherapy, a regenerative injection therapy, can be quite useful for those with spine instability. By injecting a solution into the affected ligaments and tendons, prolotherapy aims to promote tissue healing, strengthen the supporting structures, and reduce headache symptoms.
Prolotherapy for Addressing Spinal Instability and Cervicogenic Headaches
Prolotherapy, also known as regenerative injection therapy, has been a successful treatment option for cervicogenic headaches. Prolotherapy promotes tissue healing, reduces chronic inflammation, and strengthens the supporting structures in the cervical spine. Here’s an overview of the use of prolotherapy for cervicogenic headaches:
- Mechanism of Action: Prolotherapy involves injecting a solution, typically containing dextrose (a type of sugar), into the affected ligaments, tendons, or joint spaces. The solution triggers a localized inflammatory response, stimulating the body’s natural healing mechanisms. The inflammation leads to increased blood flow, collagen production, and the recruitment of cells involved in tissue repair. The goal of prolotherapy is to strengthen and stabilize the damaged or weakened structures in the cervical spine, thereby reducing cervicogenic headache symptoms. Substance such as platelet rich plasma (PRP) may be used for prolotherapy treatments.
- Potential Benefits:
- Tissue Healing: Prolotherapy aims to promote tissue healing by stimulating the production of new collagen fibers, which can strengthen ligaments and tendons in the cervical spine. This may help address the underlying causes of cervicogenic headaches.
- Pain Reduction: By strengthening the supporting structures of the cervical spine, prolotherapy may help reduce pain associated with cervicogenic headaches. It targets the source of pain and inflammation, potentially providing long-term relief.
- Clinical Evidence: While research specifically focusing on prolotherapy for cervicogenic headaches is limited, studies have explored its use in related conditions, such as chronic neck pain and whiplash-associated disorders. These studies have shown some promising results:
- A pilot study published in the Journal of Alternative and Complementary Medicine (2005) reported that prolotherapy injections significantly reduced pain and disability in patients with chronic neck pain.
- Another study published in The Clinical Journal of Pain (2005) found that prolotherapy injections resulted in significant pain reduction and improved function in patients with chronic whiplash-associated disorders.
In addition to these studies that provide preliminary evidence of the benefits of prolotherapy for neck-related conditions, there are even more first-person testimonial evidence from patients who have found relief through prolotherapy.
If you are considering prolotherapy for cervicogenic headaches, it is crucial to consult with a qualified healthcare professional who has experience in regenerative medicine and prolotherapy. They can evaluate your condition, provide an accurate diagnosis, and determine if prolotherapy is a suitable treatment option for you. Individualized treatment plans are essential to address the specific underlying causes of cervicogenic headaches and to ensure the safest and most effective approach.
Conclusion:
Cervicogenic headaches caused by spine instability can be debilitating and disrupt daily life. Understanding the relationship between spine instability and headache symptoms is crucial for effective treatment. By addressing the underlying spine instability through physical therapy, manual therapy, postural correction, and potentially prolotherapy, individuals suffering from cervicogenic headaches can find relief and improve their overall quality of life.
Find out if you’re a good candidate for prolotherapy for spinal instability by texting or calling us at 844.GO.PROLO / 844.467.7656 or send us an email at contactus@wozwellness.com
Here are some sources that you can explore for more information on cervicogenic headaches and spine instability:
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 1998;38(6):442-445. doi:10.1046/j.1526-4610.1998.3806442.x
- Biondi DM. Cervicogenic headache: a review of diagnostic and treatment strategies. J Am Osteopath Assoc. 2005;105(4 Suppl 2):16S-22S. Available at: https://jaoa.org/article.aspx?articleid=2093089
- Vincent MB. Cervicogenic headache: a comparison with migraine. Curr Pain Headache Rep. 2011;15(3):207-212. doi:10.1007/s11916-011-0180-7
- Peterson CK, Schmid C, Leemann S, et al. Outcomes from magnetic resonance imaging-confirmed symptomatic cervical disk herniation patients treated with high-velocity, low-amplitude spinal manipulative therapy: a prospective cohort study with 3-month follow-up. J Manipulative Physiol Ther. 2013;36(8):461-467. doi:10.1016/j.jmpt.2013.08.003
- Laimi K, Malmivaara A, Kalliomäki ML, et al. Effects of proprioceptive training on pain and function in chronic neck-shoulder pain patients: A randomized controlled trial. J Rehabil Med. 2019;51(9):671-679. doi:10.2340/16501977-2590
- Cusi M, Saunders J, Hungerford B, Wisbey-Roth T. The use of prolotherapy in the sacroiliac joint. Br J Sports Med. 2010;44(2):100-104. doi:10.1136/bjsm.2008.052712
- Dagenais S, Yelland MJ, Del Mar C, Schoene ML. Prolotherapy injections for chronic low-back pain. Cochrane Database Syst Rev. 2007;(2):CD004059. doi:10.1002/14651858.CD004059.pub3
- Cusi M, Saunders J, Hungerford B, Wisbey-Roth T. The use of prolotherapy in the sacroiliac joint. Br J Sports Med. 2010;44(2):100-104. doi:10.1136/bjsm.2008.052712
- Kim SR, Stitik TP, Foye PM, et al. Critical review of prolotherapy for osteoarthritis, low back pain, and other musculoskeletal conditions: a physiatric perspective. Am J Phys Med Rehabil. 2005;84(5):379-390. doi:10.1097/01.phm.0000163707.69480.aa
- Hauser RA, Hauser MA. Dextrose Prolotherapy for Unresolved Knee Pain. Practical Pain Management. 2007;7(8):56-69. Available at: https://www.practicalpainmanagement.com/pain/other/prolotherapy/dextrose-prolotherapy-unresolved-knee-pain
- Rabago D, Best TM, Beamsley M, Patterson J. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med. 2005;15(5):376-380. doi:10.1097/01.jsm.0000171301.54183.aa
- Peterson CK, Schmid C, Leemann S, et al. Outcomes from magnetic resonance imaging-confirmed symptomatic cervical disk herniation patients treated with high-velocity, low-amplitude spinal manipulative therapy: a prospective cohort study with 3-month follow-up. J Manipulative Physiol Ther. 2013;36(8):461-467. doi:10.1016/j.jmpt.2013.08.003
- Kayfetz D, Stockard AR, Beatty S, et al. Dextrose prolotherapy for recalcitrant coccygodynia. Pain Physician. 2009;12(3):E59-E66. Available at: https://www.painphysicianjournal.com/current/pdf?article=MTMzOA%3D%3D&journal=44
